Innovative Approaches to Pupil Evaluation in Neurology
Neurology is a clinical specialty that focuses on diagnosing and treating nervous system disorders. Neurologists are uniquely positioned to evaluate patients from every angle—literally! Besides evaluating neurological function through history and physical exams, many neurologists utilize tests like imaging or electrodiagnostic studies (e.g., EMG or NCS) to arrive at a complete diagnosis.
This can be important when dealing with diseases affecting multiple systems within the body, such as Alzheimer’s disease or multiple sclerosis (MS). However, not all neurologists rely solely on objective test results during a neuro exam; some may also use subjective measures such as patient-generated rating scales when conducting their evaluations.
The Limitations of Traditional Pupil Evaluation
While pupil evaluation is integral to the neurologic examination, it is not without limitations. Traditionally, pupil assessment has been based on subjective observations by the clinician and may be affected by factors such as ambient light, illumination, and magnification methods used during the examination. In addition, there is no universally accepted standard for measuring pupillary size; therefore, inter-rater reliability of pupil evaluation can be limited when using various techniques.
The lack of objectivity in pupillary evaluation contributes to other problems with consistency and precision:
- Inconsistent criteria used to define abnormality—different observers may disagree about whether a pupil change represents true pathology;
- Lack of reproducibility due to variability between examiners
Lack of objective data
The human eye is not a reliable tool for pupil evaluation.
Humans are not objective observers and may not be able to accurately assess pupil size. Pupil size can vary significantly depending on age, health, and eye position. Besides these sources of error in human observation, there is also concern about bias resulting from training or experience.
The lack of objective data makes it difficult for physicians to interpret results from pupil measurement tests correctly; this leads many doctors to rely solely on their own experience when making clinical decisions regarding diagnosis and treatment options for patients with neurological disorders such as Parkinson’s disease or Alzheimer’s Disease (AD).
Innovative Approaches to Pupil Evaluation
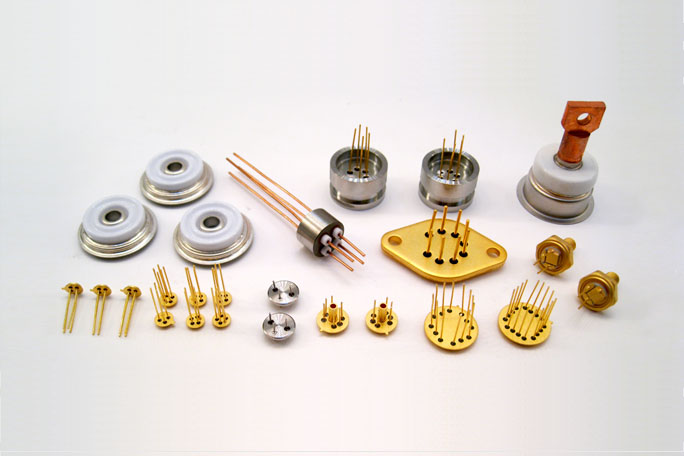
Using wearable technology, such as Google Glass, has become a common practice in neurology. Using camera-equipped glasses allows for quick and accurate pupil evaluation without touching the patient or moving them from their current position. In addition, artificial intelligence (AI) has been used as one of the neurological tools for pupil evaluation that is both cost-effective and efficient.
AI can analyze images from cameras with a minimal human intervention needed for analysis; however, there are some disadvantages associated with this method, including a lack of consistency due to different lighting conditions or angles throughout testing sessions.
Use of pupilometry
NPi pupilometry is a method of measuring the diameter of the pupil. It’s used to measure how large the pupil is, and this can be helpful when diagnosing neurological disorders, especially ones that affect vision. The size of a patient’s pupils is an essential part of a neurological exam, so it’s helpful for doctors to have a way to calculate them without relying on subjective data like patient descriptions or visual observations (which could be biased).
Pupilometry has several benefits over traditional methods:
- Objectivity: Machines measure pupils rather than being observed by humans, so there’s less room for error when recording data from multiple patients at once; no matter who does it or when it happens, there will always be consistent results because they’re based on objective measurements rather than subjective opinions about what looks normal or abnormal.
- Consistency: Because pupilometry uses machines instead of humans as observers, there isn’t any variation between different people doing similar tasks; each person will get the same result regardless of whether they’re experienced professionals or just starting.
- Ability To Capture Precise Data: When using traditional methods such as clinical observation alone then, measurements may vary depending on how well-trained individual observers are at spotting signs such as constriction/dilation patterns within their field-of-view versus outside peripheral vision, etc., whereas machine recordings produce consistent results regardless where precisely someone places themselves relative to the object being measured
Conclusion:
Many innovative pupil evaluation approaches can improve this critical test’s accuracy and efficiency. Artificial intelligence will play a vital role in this process by providing doctors with an automated means of analyzing data from wearable devices and other sources. As more hospitals adopt these technologies, we expect better patient outcomes everywhere!


.jpeg?width=682&height=455&name=AdobeStock_295048993%20(1).jpeg)

